Explore the World's Best Ideas
Join today and uncover 100+ curated journeys from 50+ topics. Unlock access to our mobile app with extensive features.
Body Dysmorphic Disorder (BDD)
BDD is a mental disorder where a person is preoccupied with an imagined or minor physical defect that others often cannot see.
As a result, people with BDD see themselves as "ugly" and often avoid social exposure. The preoccupation with the defect often leads to ritualistic behaviours, such as always looking in a mirror or picking at the skin. The person with BDD eventually becomes overly obsessed with the defect so that their social, work, and home functioning suffers.
82
814 reads
Body Dysmorphic Disorder: Common areas of concern
The most common areas of concern include:
- Skin imperfections: Wrinkles, scars, acne, and blemishes.
- Hair: Including head or body hair or absence of hair.
- Facial features: It often involves the nose but might involve the shape and size of any feature.
- Bodyweight: Sufferers may obsess about their weight or muscle tone.
Other areas of concern include the size of the penis, muscles, breasts, thighs, buttocks, and body odours.
70
459 reads
Warning signs of Body Dysmorphic Disorder
- Engaging in repetitive behaviours, such as looking in a mirror, picking at the skin, trying to cover up the perceived defect.
- Continually asking for reassurance that the defect is not too noticeable.
- Repeatedly measuring or touching the perceived defect.
- Experiencing problems at school or work, or in relationships, due to the inability to stop focusing on the perceived defect.
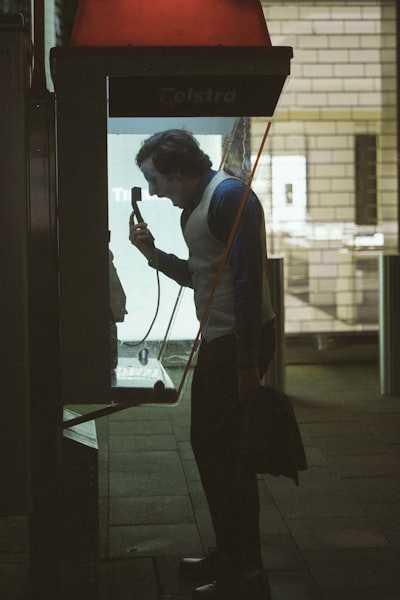
- Feeling self-conscious and not wanting to go out in public.
- Repeatedly consulting medical specialists to find ways to improve their appearance.
73
312 reads
Causes of Body Dysmorphic Disorder
One theory suggests BDD involves a problem with the size or functioning of specific brain areas. BDD often occurs in people with other mental disorders, such as major depression and anxiety.
Other factors that trigger BDD include:
- Experience of traumatic events or emotional conflict in childhood.
- Low self-esteem.
- Parents and others who were critical of the person's appearance.
- Pressure from peers and society that equates physical appearance with beauty and value.
70
267 reads
Treatment of Body Dysmorphic Disorder
Many BDD cases go unrecognised because people with the disorder often feel embarrassed and reluctant to speak about their concerns.
Treatment for BDD includes a combination of the following therapies:
- Psychotherapy. Individual counselling focuses on changing the thinking and behaviour of a person with BDD.
- Medication. Certain antidepressant medications called SSRIs are showing promise, as are antipsychotic medicines.
- Group and/or family therapy.
68
284 reads
Body Dysmorphic Disorder: The outlook is promising
The outlook is promising for people with BDD who receive and follow treatment. Those with a strong support team tend to do better in the long run.
People with BDD are at high risk for developing major depression, and the distress associated with the disorder puts people with BDD at high risk for suicide. Treatment is advisable as soon as a person begins to have symptoms. Encouraging healthy and realistic attitudes about body image is helpful, as well as a supportive environment.
66
315 reads
IDEAS CURATED BY
Charlotte 's ideas are part of this journey:
Learn more about mentalhealth with this collection
Navigating and enjoying the thrill of horror and scare experiences
Historical knowledge of Halloween and its origins
Understanding and appreciating Halloween traditions worldwide
Related collections
Similar ideas
Read & Learn
20x Faster
without
deepstash
with
deepstash
with
deepstash
Personalized microlearning
—
100+ Learning Journeys
—
Access to 200,000+ ideas
—
Access to the mobile app
—
Unlimited idea saving
—
—
Unlimited history
—
—
Unlimited listening to ideas
—
—
Downloading & offline access
—
—
Supercharge your mind with one idea per day
Enter your email and spend 1 minute every day to learn something new.
I agree to receive email updates